Malformations of Cortical Development (MCD)
Different types of MCD are recognized based on anatomy. They carry names like microcephaly (small brain and head), schizencephaly (fluid filled clefts in the brain), pachygyria (a cortex with thicker, fewer folds) and polymicrogyria (cortex with many small folds).
——————————————————————–
This information comes from the article posted at:
http://www.nih.gov/news/health/aug2010/ninds-22.htm?utm_source=twitterfeed&utm_medium=twitter
Embargoed for Release
Sunday, August 22, 2010
1 p.m. EST
Contact:
National Institute of Neurological Disorders and Stroke (NINDS)
National Center for Research Resources (NCRR)
National Institute of Mental Health (NIMH)
Gene scan finds link across array of childhood brain disorders
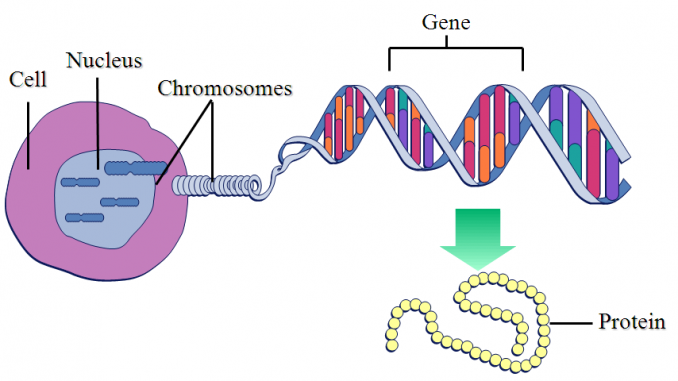
Mutations in a single gene can cause several types of developmental brain abnormalities that experts have traditionally considered different disorders. With support from the National Institutes of Health, researchers found those mutations through whole exome sequencing — a new gene scanning technology that cuts the cost and time of searching for rare mutations.
Brain scans of a healthy child (left) and a child with microcephaly, polymicrogyria and schizencephaly. Courtesy of Murat Gunel, M.D., Yale University. “This is going to change the way we approach single-gene disorders,” said lead investigator Murat Gunel, M.D., who is chief of the Neurovascular Surgery Program and co-director of the Program on Neurogenetics at Yale University in New Haven, Conn. Whole exome sequencing can be applied to dozens of other rare genetic disorders where the culprit genes have so far evaded discovery, he said.
Such information can help couples assess the risk of passing on genetic disorders to their children. It can also offer insights into disease mechanisms and treatments.
The research is funded in part by a $2.9 million stimulus grant from NIH’s National Institute of Neurological Disorders and Stroke (NINDS) made possible by the American Recovery and Reinvestment Act.
“This study demonstrates a powerful new tool for discovering the cause of tough-to-crack genetic disorders,” said NINDS director Story Landis, Ph.D. “It also exemplifies how Recovery Act support to the NIH community is successfully driving biomedical technology and innovation.”
The study appears in Nature, and focuses on children with malformations of cortical development (MCD). These are severe abnormalities of the cerebral cortex, the brain’s outermost layer, which normally contains complex folds that are densely packed with brain cells. In MCD, the cortex is smaller and its folds are less complex. Affected children have severe intellectual disabilities and may not reach developmental milestones.
Different types of MCD are recognized based on anatomy. They carry names like microcephaly (small brain and head), schizencephaly (fluid filled clefts in the brain), pachygyria (a cortex with thicker, fewer folds) and polymicrogyria (cortex with many small folds). These conditions reflect a failure of brain cells to grow and reach their proper places during development. They can result from prenatal exposure to alcohol, drugs and some viruses. In many cases, the cause is genetic, but the specific genetic lesion is often unknown.
Through whole exome sequencing, the new study found a single gene at the root of seemingly distinct types of MCD in children from multiple families. Rather than scanning a person’s entire genome for mutations, this technique focuses on the protein-coding bits of DNA, or exome, which makes up about 1.5 percent of the genome.
Genetic forms of MCD occur worldwide and in all kinds of families, but the highest incidence is among children born to parents who are related. Dr. Gunel and his colleagues at Yale teamed up with investigators in Turkey to study Turkish families with MCD. The country has a tradition of first- and second-cousin marriages, and thus a relatively high incidence of MCD.
The study began by focusing on two related children who were diagnosed with microcephaly. Whole exome sequencing revealed that both children had mutations in a gene called WDR62. As the study grew to include children from other families with microcephaly, many of the children were found to have mutations in the same gene. Unexpectedly, brain imaging revealed that the children also tended to have other types of MCD, superimposed with microcephaly. In all, the investigators found 6 unique mutations in the WDR62 gene among 30 families.
Those results show that a single gene “is required for strikingly diverse aspects of human cortical brain development,” said Dr. Gunel.
No one knows precisely what WDR62 does, but related proteins are known to regulate the processing of RNA (the intermediate between DNA and protein). The researchers found that in the developing mouse and human brain, WDR62 is enriched in a band of brain tissue that contains neural stem cells. They plan to explore the exact functions of WDR62 in mouse studies. Meanwhile, they will use their Recovery Act grant to extend whole exome sequencing to hundreds of additional families with MCD.
The technology should prove to be quick and cost effective for identifying the roots of other rare genetic disorders too, according to Dr. Gunel. In his laboratory, whole genome sequencing takes several weeks and costs about $50,000, while whole exome sequencing takes 9 days and costs about $3,500, he said.
In addition to NINDS, other support for the study came from a Clinical and Translational Science Award from NIH’s National Center for Research Resources, and from NIH’s National Institute of Mental Health.
NINDS (www.ninds.nih.gov) is the nation’s leading funder of research on the brain and nervous system. The mission of NIMH (www.nimh.nih.gov) is to reduce the burden of mental and behavioral disorders through research on mind, brain and behavior. NCRR (www.ncrr.nih.gov) provides laboratory scientists and clinical researchers with the resources and training they need to understand, detect, treat and prevent a wide range of diseases.
The National Institutes of Health (NIH) — The Nation’s Medical Research Agency — includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. It is the primary federal agency for conducting and supporting basic, clinical and translational medical research, and it investigates the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov.
The activities described in this release are being funded through the American Recovery and Reinvestment Act. More information about NIH’s Recovery Act grant funding opportunities can be found at http://grants.nih.gov/recovery/. To track the progress of HHS activities funded through the Recovery Act, visit www.hhs.gov/recovery. To track all federal funds provided through the Recovery Act, visit www.recovery.gov.
For information on Murat Gunel, M.D., see his website:
http://www.med.yale.edu/neurosur/faculty/gunel.html
Patient and Referring Physician Information
Clinical and Appointment Address:
Yale Neurosurgery
800 Howard Avenue
Yale Physicians Building-3rd Floor
New Haven, CT 06519
US Mailing Address:
Yale University School of Medicine
Department of Neurosurgery
PO BOX 208082
New Haven, CT 06520
Appointment and Office Phone: (203) 737-2096
E-mail murat.gunel@yale.edu